In the progressive stages of Alzheimer’s disease, the aggregation of amyloid proteins in the brain leads to the formation of damaging plaques, incrementally exacerbating dementia symptoms. A leading edge in altering the trajectory of Alzheimer’s involves interventions aimed at either dismantling these toxic amyloid accumulations or preventing their formation from the outset. This approach gained momentum when the US Food and Drug Administration approved a pioneering therapeutic for early-stage Alzheimer’s that mitigates cognitive decline by targeting amyloid plaques—a notable milestone, yet further advancements are crucial. As of 2023, an estimated 6.7 million Americans are confronting this relentless ailment.
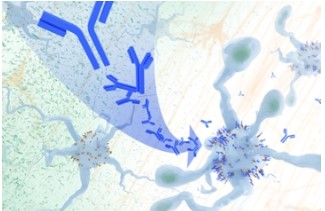
Innovative research, supported by the National Institutes of Health and spotlighted in Science Translational Medicine, delineates a fresh strategy for amyloid plaque removal in the brain, trialed in murine models. At the crux of this approach is the engagement of the brain’s inherent waste removal system: the microglial immune cells, which are instrumental in curbing Alzheimer’s progression. These findings open the door to the possibility of crafting immunotherapeutic interventions that harness the body’s immune defenses to stimulate microglia within the Alzheimer’s-affected brain, bolstering the clearance of amyloid plaques.
The investigative team, including Marco Colonna from the Washington University School of Medicine in St. Louis and Jinchao Hou, presently affiliated with the Children’s Hospital of Zhejiang University School of Medicine in Zhejiang Province, China, reported that microglia envelop plaques to form a protective barrier, attenuating their dissemination. These immune cells are also capable of directly eradicating amyloid plaques. However, their efficacy is contingent upon a delicate equilibrium of stimulatory and inhibitory signals. In individuals with Alzheimer’s, this balance is distorted, mitigating the microglia’s protective functions.
The researchers explored the possible link between Alzheimer’s disease and apolipoprotein E (APOE), a protein normally tasked with transporting fats such as cholesterol through our blood. The gene encoding APOE is notorious for affecting an individual’s likelihood of developing Alzheimer’s. Moreover, within the brain afflicted by Alzheimer’s, APOE becomes a fundamental component of the injurious amyloid plaques. It has an additional, less beneficial role, where it might deactivate microglia, the brain’s immune cells, by latching onto a receptor called LILRB4 on their surfaces.
Prior Alzheimer’s research in murine models indicated that the LILRB4 receptor presence is highly elevated in microglia amidst the proliferation of amyloid plaques. This aspect hinted that therapies aimed at this microglia receptor might be promising in the battle against Alzheimer’s. In their latest endeavor, the researchers sought signs that an uptick in LILRB4 receptors on microglia is pivotal within the brains of individuals with Alzheimer’s.
Firstly, the team analyzed brain tissue from deceased individuals who had Alzheimer’s, confirming the microglia displayed an unusually high expression of LILRB4 receptors, echoing observations from mouse models. This finding may shed light on the difficulty microglia face in reigning in amyloid plaques in Alzheimer’s-affected brains.
Subsequently, they investigated the effects of an antibody directed at the LILRB4 receptor in mouse brains rife with amyloid plaques. The results suggest the treatment disrupted the bond between APOE proteins and LILRB4 receptors, which in turn activated microglia to eradicate the plaques. The research took a fascinating turn when they observed that this removal process seemed to influence the mice’s behavior, rendering them more cautious and less prone to risk-taking. This behavioral shift is noteworthy given that individuals with Alzheimer’s often partake in risky behaviors due to a disconnection from past experiences which would typically inform safer decision-making.
The research opens new avenues of discovery. Currently, it remains unclear whether this tactic influences the tau protein, notorious for its detrimental tangles within neurons of the Alzheimer’s-affected brain. Additionally, the scientists aim to explore any potential adverse health effects that might accompany amyloid plaque removal.
Nevertheless, these recent insights contribute to the mounting evidence that immunotherapy of this nature holds potential as a therapeutic avenue for Alzheimer’s. The implications extend further, potentially influencing the treatment of other neurodegenerative disorders marked by harmful brain deposits, such as Parkinson’s disease, amyotrophic lateral sclerosis (ALS), and Huntington’s disease. The ultimate aspiration is that such investigative efforts will forge a path to more effective treatments for Alzheimer’s and similar neurological ailments.